INVOLUNTARY MOVEMENTS OF B/L UPPER AND LOWER LIMBS OF A 38y|M
38 year old male autodriver by occupation came to the casuality with chief complaints of involuntary movements of both upper and lower limbs
HISTORY OF PRESENT ILLNESS :-
patient was apparently normal. Yesterday, after consuming alcohol he started showing aggressive behaviour and developed involuntary movements of both upper and lower limbs- tonic clonic lasted for 10 mins, up rolling of eyes present, tongue bite- present, there was no post icteral confusion or involuntary micturition/defecation.
Visual and auditory hallucinations +/? Fearfulness +/?
No c/o pain abdomen,nausea,vomiting,chest pain, palpitations.
Pt is consuming alcohol since 10-12yrs (180ml/day 3-4 times a week)
PAST HISTORY
No similar complaints in the past
N/K/C/O. Dm,Htn, Epilepsy
h/o appendicectomy 10 yrs ago
GENERAL EXAMINATION
Patient was conscious, not co operative
pallor , icterus, cyanosis, clubbing, lymphadenopathy,edema are absent
vitals at the time of admission i.e 28-2-22
temp. afebrile
BP 150/100mm hg
PR 82bpm.
RR 19cpm
spo2 100 @RA
GRBS 330mg/dl
SYSTEMIC EXAMINATION
Cvs: s1 s2 heard
RS: BAE +
P/A : soft , non tender
CNS: Pt is conscious , speech is normal , no signs of meningial irritation
Cranial nerves are intact
Gait is normal
Reflexes : B T S K A P
Rt + + + + + +
Lt + + + + + +
Power: Rt Lt
UL 4/5 4/5
LL 4/5 4/5
Sensory system : able to perceive sensations normally
INVESTIGATIONS
SARS-COV-2 PCR : NEGATIVE
GRBS: 113mg/dl
BLOOD UREA:
29mg/dl
SERUM CREATININE: 1.5 mg/dl
Serum electrolytes
Na: 136
K: 3.6
Cl: 98
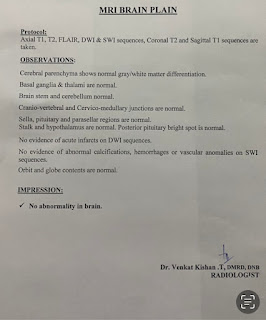
MRI : NAD
EEG:
PROVISIONAL DIAGNOSIS
Seizure under evaluation
Alcohol withdrawal ?
TREATMENT
1. Inj LEVIPIL 500mg IV / BD
2. inj OPTINEURON 1amp in 100ml NS IV
3. Inj. THIAMINE 1amp in 100 ml NS IV / TID
4. INJ LORAZEPAM 4mg IV /sos
5.inj pantop 40 mg iv /bd
6.inj zofer 4 mg iv /sos
1-3-22
Pt is c/c
BP:110/80 mm Hg
PR: 80bpm
CVS: s1 s2 heard
RS: BAE +
GRBS:113mg/dl
TREATMENT:
1) T. LEVIPIL 500MG
2) INJ. THIAMINE 100MG IV BD
3) ZYTER GEL for L/A on tongue
4) INJ PAN 40MG IV OD
5) INJ ZOFER 4MG IV SOS
2-3-22
Pt is c/c
Vitals are stable
TREATMENT:
1) T. LEVIPIL 500MG
2) INJ. THIAMINE 100MG IV BD
3) ZYTER GEL for L/A on tongue
4) INJ PAN 40MG IV OD
5) INJ ZOFER 4MG IV SOS







Comments
Post a Comment